Simplifying Decision-Making with Real-Time Payers Data Analytics
Whether you are looking to contain costs, improve employee engagement, or increase quality of process, analytics plays a vital role in achieving these objectives. Our proven analytic solutions help you harness vast amounts of data flowing through your organization, enabling insight-driven operations, enhancing efficiencies, and driving clinical/business value.
What Problem Can We Solve?
Leverage a one-stop solution like InsightPro to handle everything quickly and easily
OR
Why MDI NetworX?
We offer the right suite of solutions for the post-pandemic challenges that healthcare payers face. Our intelligent solutions can help you beat the odds faster.
Digital Intake
Automation is the answer to increased customer expectations, reduced staff, and lowered administrative costs. Going digital can improve efficiency and productivity.
Core Admin Solutions
Businesses like yours need to continue to offer the same levels of services with fewer personnel. Let us automate your core admin responsibilities.
Digital Mailroom & Fulfillment
Our cost-effective mailroom management software will increase productivity in your organization through scanning solutions and more.
Our Products
Our products emerge from a deep understanding of the challenges faced by healthcare payers today with a suite of proven solutions geared to tackle those challenges head on.
InsightPro
This customizable tool is designed to enhance efficiency and performance across your operations.
Know More
RevEx
RevEx is an advanced Revenue Cycle Management platform crafted to streamline & optimize healthcare billing processes.
Know More
Golem
As a frontend claims processing solution, Golem offers an elegant interface for a seamless backend workflow.
Know More
Docgem
Using automation, this tool handles the critical tasks of record access, confidentiality, workflow distribution, and reporting.
Know More
MCO PRO
This fully-automated PPO routing and repricing application performs tasks efficiently and with complete transparency, which can be accessed any time during the claim process.
Know More
Mage
This tool will reduce time, cost, and effort in preparing and negotiating contracts that are financially viable to providers.
Know More
Our Solutions
We work with our clients to manage the more mundane responsibilities of business, giving their team more time
to focus on their core capabilities.
All
Payers
Providers
Procurement
Heathcare Procurement
Achieve cost control and compliance with our strategic, end-to-end procurement services. From sourcing to payment, streamline operations and strengthen supplier partnerships.
Know moreClaims Administration
With our experienced onshore and offshore claims adjudication and adjustment professionals, healthcare payers and TPAs are assured faster settlements, better accuracy and lower processing costs per claim.
Know moreProvider Call Center
With advanced technology and experienced agents, we optimize communication channels and improve operational efficiency. Trust MDI NetworX as your Provider Call Center partner to enhance patient care and streamline your organization's communication needs.
Know moreRevenue Cycle Management
Our Revenue Cycle Management (RCM) solution is designed to address the complexchallenges healthcare providers face in managing their finances effectively.
Know more
![]()
Practice Management
Enhance efficiency and compliance with our customized practice management solutions. Streamline financials, credentialing, and IT support seamlessly.
Know more![]()
Payer Administrative Services
Streamline operations and boost member satisfaction with our expert Payer Administrative Services, featuring precise compensation management and advanced tech integration.
Know moreDigital Mailroom Management
Take advantage of our ultra-modern technology that brings to you exceptional mailroom and scanning solutions and gives your operations the benefit of OCR ready (300 DPI) images.
Know moreData Capture
ML/AI is put to good use via Optical Character Recognition (OCR) and Intelligent Character Recognition (ICR) technologies. This helps you capture data from printed as well as hand-written forms and correspondence documents, and convert them into EDI.
Know moreMember Enrollment
Healthcare payers and related third party administrators can discover high-quality member enrollment, premium billing, eligibility support and member fulfilment solutions.
Know moreBusiness Rule Configuration
Allow our experienced and certified configuration analysts to use their skills and help you configure benefit plans, pricing, provider network, etc. on all the popular claims administration platforms.
Know moreQuality Assurance
Improve the overall efficiency of your operations with our 1st Pass and 2nd Pass audit solutions that can help you meet the solution levels of claims and also provide re-training triggers.
Know moreReporting & Analytics
Our team of experienced and qualified MIS analysts and reporting specialists can take your complicated reporting tasks and turn in finished reports within the stipulated turnaround time.
Know moreNo Surprises Act
As the US healthcare arena gets ready for the No Surprises Act, we will help you navigate this changing landscape with our expert manpower and years of experience.
Know moreManaged Services
We have a strong focus on emerging technologies and towards that we invest in the latest tech innovation to facilitate high-quality tech solutions for our clients.
Know moreOur Resources
Our leaders have a wealth of knowledge to share with clients and partners.
InsightPro,
MDI's Flagship Offering
Our healthcare insurance payer operations cover a gamut of services, including high-quality Services, Consultation and IT Solutions. We are committed to providing exceptional services that meet the exact needs of healthcare payers, and towards that we deploy the latest technologies.
Know More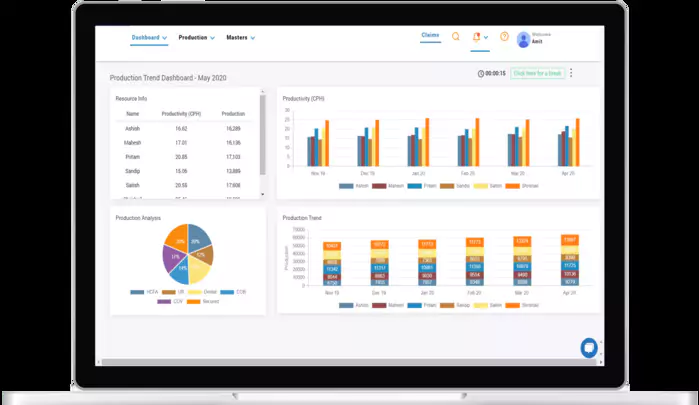
Client Testimonials
Hear what our clients have to say about working with MDI NetworX.
I just wanted to take a moment to share some feedback that I have been receiving from my Claims leads (and some of my own) that your team works with on a day-to-day basis. I have consistently received the feedback that your team is responsive, meticulous in the work, and constantly polite
I wanted to thank you and the team for the excellent work that you are doing for the Accumulator Requests. You were able to beat the committed completion dates, which is very much appreciated. Please share my appreciation with the team! Great work and thank you!
You have been doing a great job with all the extra stuff we have been sending your way like the special claims and the stop loss claims plus the claims that need 3 or 4 levels of audit. Thank you and your team for always stepping up and helping out.
Our Certifications
All our products and services are certified by reputed worldwide organizations.



Join MDI
If you’re looking for a fast-paced career with numerous rewards and recognitions, then join MDI NetworX today
Search and apply


